Following up on our review of the bariatric surgical procedures currently available let's take a closer look at sleeve gastrectomy or The Sleeve, or VSG.
In the vernacular language of weight loss surgery wearing a sleeve has nothing to do with a piece of clothing that covers the arm; wearing a sleeve describes a relatively new surgical procedure that is fast gaining favor for the treatment of morbid obesity. The procedure involves removing a portion of the stomach and the formation of a tubular stomach sleeve different in shape and function from the more common gastric bypass pouch. This procedure restricts food intake but is not considered malabsorptive which often results in dumping syndrome and vitamin deficiency in gastric bypass patients. It is believed that the sleeve procedure also reduces the amount of ghrelin and other hormones that are released providing a hormonal advantage to reducing caloric intake.
According to Dr. Gregg H. Jossart, Director of Minimally Invasive Surgery at California Pacific Medical Center, the sleeve gastrectomy is an evolution of prior procedures that has its roots in the earliest bariatric weight loss surgery procedures. The first open sleeve gastrectomy was performed in March 1988 as part of what is now called the duodenal switch procedure. By 2001 the open sleeve gastrecomy was increasingly used for treating super morbidly obese patients who were deemed too high risk for other metabolic weight loss surgeries such as gastric bypass or the duodenal switch. Doctors were seeing patients achieve a weight loss of 40 to 50 percent excess weight. Once the super morbidly obese patient achieved this initial weight loss they could undergo a "second stage" procedure, most likely the Roux-en-Y gastric bypass surgery, which brought continued weight loss.
In the meantime advances were being made in laparoscopic gastric surgeries that were reducing risk to patients and decreasing hospital stays while improving the rate of recovery from surgery. Minimally invasive laparoscopic procedures are performed by surgeons inserting cameras and instruments through small incisions using images displayed on high resolution monitors for magnification of the surgical elements.
Super-morbidly obese patients, those with a BMI greater than 58, are not always suited to laparoscopic bariatric surgical procedures due to the depth of adipose tissue. But techniques were developed by 2003 that made a laparoscopic approach to the sleeve feasible. A small study of super morbidly obese patients undergoing the laparoscopic sleeve gastrectomy indicated an average excessive weight loss of 33 percent. These patients were then able to safely undergo the second stage Roux-en-Y gastric bypass surgery, also laparoscopically.
By 2009 several study groups at different stages post-surgery were all reporting favorable weight loss with the laparoscopic sleeve gastrectomy. The results were so favorable in fact, results in weight loss were comparable to both gastric bypass and adjustable gastric banding. These results quickly popularized the procedure for patients seeking surgical intervention for the metabolic disorder of morbid obesity.
Todays laparoscopic sleeve gastrectomy, which evolved from an open duodenal switch to open sleeve gastrectomy, is fast becoming the favored procedure for super-morbidly obese patients as the first stage operation before Roux-en-Y. For patients of lower BMI the sleeve procedure is effective as a single treatment for weight loss and presents another surgical option to the better known gastric bypass or adjustable gastric band (lap-band) surgeries. Bariatric surgeons are happily reporting that the long-term safety of the sleeve procedure is definite as the risk of marginal ulcer or small intestinal obstruction does not exist as it does with gastric bypass.
However, surgeons are seeking to resolve two main issues with the gastric sleeve. The first is a standardized pouch volume. It is believed a smaller pouch volume of 30-40cc will affect a more durable weight loss, but with this smaller volume comes problems. Jossart said, "Unfortunately this smaller volume increases the chance of staple line bleeding or splitting, especially near the gastroesophageal junction. Proper management of the staple line will ultimately optimize the safety of this procedure."
As with all surgical procedures it is critical to have the surgery performed by a board-certified surgeon who is familiar with the anatomy, surgical procedure, and postoperative management of the patient.
Want to talk about your procedure? Join us in our Facebook group: LivingAfterWLS Project 2014.
The LivingAfterWLS blog is now 12-years old, one of the oldest and most consistent WLS blogs in the Blogsphere. We strive to provide current, unbiased information for the improvement of health & wellness after WLS. Thank you for joining us! This blog is an official satellite of the websites LivingAfterWLS.com; LAWLSBookstore.com & 5DayPouchTest.com. Our ongoing research is funded by affiliate links & proceeds from our publications. We appreciate your patronage.
Thursday, August 21, 2014
Putting Up: Dilly Beans
 |
| Dilly Beans by Kaye Bailey |
From Crafting with KeepHer & Kaye
I've been making Dilly Beans for at least a dozen years, give or take a missed season here and there. Last year my beans went bad while we attended a family issue. It was sad to see my dilly bean shelf empty all winter. Dilly beans are the perfect addition to a veggie tray that includes pickles and olives. And when the guys get together for a poker game my Dilly's are on the top of the request list.The local farm stand is open here on Wednesdays. I arrived there early and the green beans were at the peak of the season. So Dilly Beans it was. I've been using the recipe from Ball Blue Book all these years (see original recipe below) and made a few tweaks to suit our taste. More garlic. Red pepper flakes in place of the cayenne. A pinch of celery seed. And just for prettiness sake I add a few matchsticks of carrot or bell pepper. Why bother with canning if it doesn't look lovely on the shelf?
Dilly Beans benefit from a three to four month curing period, stored properly out of sunlight in a cool room.
The following is the original recipe from Ball Blue Book. Be sure to following strict canning and processing procedures to ensure the safety and goodness of your put-up produce.
Original Dilly Bean Recipe
Original recipe (C) Ball Blue Book 1997 by Alltrista Corporation.
1997 by Alltrista Corporation.
Ingredients:
2 pounds green beans
1/4 cup canning salt
2-1/2 cups white vinegar
2-1/2 cups water
1 teaspoon cayenne pepper, divided
4 cloves garlic, divided
4 heads dill, divided
Directions:
Trim ends off green beans. Combine salt, vinegar, and water in a 2-quart sauce pan. Bring to boil. Pack beans lengthwise into hot jars, leaving 1/4-inch headspace. Add 1/4 teaspoon cayenne pepper, 1 clove garlic, and 1 head dill to each pint. (For quarts add 1/2 teaspoon cayenne pepper, 2 cloves garlic, and 2 heads dill to each jar with the green beans.) Ladle hot liquid over beans, leaving 1/4-inch headspace. Remove air bubbles. Adjust two-piece caps. Process pints and quarts 10 minutes in a boiling water canner.
Yield: about 4 pints or 2 quarts
Ingredients:
2 pounds green beans
1/4 cup canning salt
2-1/2 cups white vinegar
2-1/2 cups water
1 teaspoon cayenne pepper, divided
4 cloves garlic, divided
4 heads dill, divided
Directions:
Trim ends off green beans. Combine salt, vinegar, and water in a 2-quart sauce pan. Bring to boil. Pack beans lengthwise into hot jars, leaving 1/4-inch headspace. Add 1/4 teaspoon cayenne pepper, 1 clove garlic, and 1 head dill to each pint. (For quarts add 1/2 teaspoon cayenne pepper, 2 cloves garlic, and 2 heads dill to each jar with the green beans.) Ladle hot liquid over beans, leaving 1/4-inch headspace. Remove air bubbles. Adjust two-piece caps. Process pints and quarts 10 minutes in a boiling water canner.
Yield: about 4 pints or 2 quarts
Tuesday, August 19, 2014
Back to School Week: Get your LAWLS books on Kindle & Save
Kindle editions as low as $8.95
Shop Amazon for all your LivingAfterWLS publications! See our storefront
Shop Amazon for all your LivingAfterWLS publications! See our storefront
Bariatric Weight Loss Procedures and the Names They Go By
It's Back to School week here at LivingAfterWLS! I love this time of year - new starts, refresher studies, and back to the art and craft of learning. Yesterday we reviewed the Four Rules of bariatric weight loss surgery. Today, for anyone considering weight loss surgery, for new patients or veterans of surgical weight management I present a brief review of the currently approved surgical procedures and the names they go by.
By Kaye Bailey
The advisory committee for the 2010 Dietary Guidelines for Americans reported grim news earlier this year when they confirmed that currently about two-thirds of American adults and one-third of American children are overweight or obese. The committee warned that Americans must slash their caloric intake and increase physical activity because the obesity epidemic is "the single greatest threat to public health in this century."
Given that discouraging news nearly 300,000 adult Americans will undergo bariatric surgery this year as a means to losing weight and treating chronic morbid obesity. There are at least 35 bariatric surgical procedures approved by the Food and Drug Administration (FDA) for the treatment of obesity. While each procedure is unique they are all generically referred to as Weight Loss Surgery (WLS). The American Society for Metabolic and Bariatric Surgery describes two basic approaches that weight loss surgery takes to achieve change:
Gastric Bypass Surgery: Since the early 1990s gastric bypass has been the most commonly performed surgical weight loss procedure and the laparoscopic gastric bypass is considered the "gold standard" of bariatric surgery. The public at large often mistakenly calls all bariatric procedures gastric bypass. Gastric bypass is both a restrictive and malabsorptive procedure. Patients refer to it as WLS, GBS, Roux-en-Y Gastric Bypass (RYGB) or simply gastric bypass.
Adjustable Gastric Banding: This procedure, most commonly called lap-band, is restrictive with the use of a prosthetic band placed around the upper part of the stomach, much like a belt. There is no cutting or stapling of the stomach. A tube is connected to the prosthetic band to a small access port that is fixed beneath the abdomen skin. The band is adjusted through this port to help control weight loss outcome. Patients call this procedure banding, lap-band, or gastric banding. They refer to themselves as "Bandsters" or "Bandits".
Sleeve Gastrectomy: This is a purely restrictive procedure meaning there is no intestinal bypass. The sleeve gastrectomy is rapidly emerging as a reasonable alternative to adjustable gastric banding and other stapling procedures with patients favoring it over the malabsorptive procedures. Among patients the procedure is often called "gastric sleeve" or "the sleeve" and patients of this procedure refer to themselves as "sleevesters".
Laparoscopic vs. Open Procedure: Laparoscopic procedures are used for a variety of general surgeries and in the last decade have become the predominant technique for many surgical procedures. When a laparoscopic operation is performed a small video camera is inserted into the abdomen through small incisions made in the abdominal wall. The surgeon views the procedure on a separate video monitor. Laparoscopic procedures are considered less invasive than open procedures that require one long incision to open the abdomen. Studies indicate patients having had laparoscopic weight loss surgery experience less pain after surgery resulting in easier breathing and lung function and higher overall oxygen levels. In addition laparoscopy patients have fewer wound complications such as infection or hernia, and they tend to return to quickly to pre-surgical levels of activity.
Kaye Bailey (c) 2010 - All Rights Reserved
To learn how to make the most of these procedures,
take a look at this featured article from the 5 Day Pouch Test website:
By Kaye Bailey
The advisory committee for the 2010 Dietary Guidelines for Americans reported grim news earlier this year when they confirmed that currently about two-thirds of American adults and one-third of American children are overweight or obese. The committee warned that Americans must slash their caloric intake and increase physical activity because the obesity epidemic is "the single greatest threat to public health in this century."
Given that discouraging news nearly 300,000 adult Americans will undergo bariatric surgery this year as a means to losing weight and treating chronic morbid obesity. There are at least 35 bariatric surgical procedures approved by the Food and Drug Administration (FDA) for the treatment of obesity. While each procedure is unique they are all generically referred to as Weight Loss Surgery (WLS). The American Society for Metabolic and Bariatric Surgery describes two basic approaches that weight loss surgery takes to achieve change:
Restrictive procedures that decrease food intake with the use of stapling or banding.
Malabsorptive procedures that alter digestion causing food to be poorly digested and incompletely absorbed so that it is eliminated in the stool.Patients seeking surgical help for obesity quickly learn the nomenclature of bariatric medicine and can readily list the names by which different surgical procedures are known. Bariatric procedures are all effective in the treatment of morbid obesity, but differ in degree of weight loss and range of complications. The choice of procedure, according to the European Association for Endoscopic Surgery, should be tailored to the individual situation. Here we look at the most commonly performed bariatric procedures in the United States and learn the names they go by:
Gastric Bypass Surgery: Since the early 1990s gastric bypass has been the most commonly performed surgical weight loss procedure and the laparoscopic gastric bypass is considered the "gold standard" of bariatric surgery. The public at large often mistakenly calls all bariatric procedures gastric bypass. Gastric bypass is both a restrictive and malabsorptive procedure. Patients refer to it as WLS, GBS, Roux-en-Y Gastric Bypass (RYGB) or simply gastric bypass.
Adjustable Gastric Banding: This procedure, most commonly called lap-band, is restrictive with the use of a prosthetic band placed around the upper part of the stomach, much like a belt. There is no cutting or stapling of the stomach. A tube is connected to the prosthetic band to a small access port that is fixed beneath the abdomen skin. The band is adjusted through this port to help control weight loss outcome. Patients call this procedure banding, lap-band, or gastric banding. They refer to themselves as "Bandsters" or "Bandits".
Sleeve Gastrectomy: This is a purely restrictive procedure meaning there is no intestinal bypass. The sleeve gastrectomy is rapidly emerging as a reasonable alternative to adjustable gastric banding and other stapling procedures with patients favoring it over the malabsorptive procedures. Among patients the procedure is often called "gastric sleeve" or "the sleeve" and patients of this procedure refer to themselves as "sleevesters".
Laparoscopic vs. Open Procedure: Laparoscopic procedures are used for a variety of general surgeries and in the last decade have become the predominant technique for many surgical procedures. When a laparoscopic operation is performed a small video camera is inserted into the abdomen through small incisions made in the abdominal wall. The surgeon views the procedure on a separate video monitor. Laparoscopic procedures are considered less invasive than open procedures that require one long incision to open the abdomen. Studies indicate patients having had laparoscopic weight loss surgery experience less pain after surgery resulting in easier breathing and lung function and higher overall oxygen levels. In addition laparoscopy patients have fewer wound complications such as infection or hernia, and they tend to return to quickly to pre-surgical levels of activity.
Kaye Bailey (c) 2010 - All Rights Reserved
To learn how to make the most of these procedures,
take a look at this featured article from the 5 Day Pouch Test website:
Three Keys to Lasting Weight Loss Surgery Success
Nearly a quarter-million people in the United States will undergo weight loss surgery this year to arrest their morbid obesity and lose weight. In spite of the drastic nature of gastric surgeries not all patients will reach a healthy weight and some may eventually regain weight they lost initially with surgery. Read moreMonday, August 18, 2014
Back to School Week: The Four Rules
Weight loss surgery (WLS) is frequently perceived as an easy means to weight loss that requires little or no effort by the patient. However, patients who undergo bariatric surgery are prescribed Four Rules of dietary and lifestyle management that they will follow for the rest of their life if they wish to lose weight and maintain a healthy weight. All surgical weight loss procedures including gastric bypass, adjustable gastric banding (lap-band) and gastric sleeve, promote weight loss by decreasing energy (caloric) intake with a reduced or restricted stomach size. The small stomach pouch is only effective when a patient rigorously follows the Four Rules: eat a high protein diet; drink lots of water; avoid snacking on empty calorie snack foods; engage in daily exercise.
As part of their introduction to a bariatric program most patients are taught the Four Rules, which tend to be consistent from one bariatric program to the next. Many patients agree to follow the Four Rules which will work in concert with their surgically altered stomach and digestive system to bring about rapid massive weight loss. Some patients mistakenly believe they can return to the eating and lifestyle habits they practiced before surgery once they have lost the desired amount of weight. However, patients who return to their pre-surgery lifestyle and diet often fail to achieve full body fat loss and frequently regain much of the weight they initially lost.
For patients to lose all of their excess weight and maintain that weight loss they must follow the Four Rules for the rest of their life. Before undergoing any surgical procedure for weight management one must be fully aware of the Four Rules and willing to commit to them for life. Below is a quick look at each rule as it applies to WLS patients:
Protein First: At every meal the WLS patient will eat lean animal, dairy, or vegetable protein before any other food. Protein shakes or supplements may be included as part of the weight loss surgery diet. Patients are advised to consume 60-100 grams of protein a day. Eating lean protein will create a tight feeling in the surgical stomach pouch: this feeling is the signal to stop eating. Many patients report discomfort when eating lean protein, yet this discomfort is the very reason the stomach pouch is effective in lowering energy intake. Patients should not consume liquids while eating solid food because liquids will cause the stomach pouch to empty too quickly preventing nutrient absorption and satiation.
Lots of Water: Like most weight loss programs, bariatric surgery patients are instructed to drink lots of water throughout the day. Water hydrates the organs and cells and facilitates the metabolic processes of human life. Water flushes toxins and waste from the body. Patients are prohibited carbonated beverages and advised to drink caffeinated or alcoholic beverages sparingly.
No Snacking: Patients are discouraged from snacking which may prevent weight loss and lead to weight gain. Specifically, patients are forbidden to partake of traditional processed carbohydrate snacks, such as chips, crackers, baked goods, and sweets. Patients who return to snacking or grazing defeat the restrictive nature of the surgery and weight gain results.
Daily Exercise: Patients in recovery from morbid obesity must increase their daily activity and progress to formal fitness building activities that include aerobic conditioning and muscular strength and endurance. Walking, swimming, and biking are all encouraged following gastric surgery. Patients who continue to follow an exercise routine will sustain weight loss and live healthier lives. Patients who do not include exercise as part of their bariatric weight loss program will most likely regain weight and suffer from co-morbidities they hoped to relieve with surgical weight loss.
Nearly a half-million Americans this year will undergo some form of bariatric surgery for the treatment of their morbid obesity. Surgical intervention is proven to be the best treatment for many people in affecting long term weight loss and weight management. However, surgery does not work alone. Patients who are compliant with the Four Rules of dietary and lifestyle change are most likely to enjoy improved health and mobility following a bariatric intervention.
Learn more about the Four Rules and get back to the basics of WLS with the 5 Day Pouch Test plan. Check out the Owner's Manual available for instant download on Kindle:
5DPT Owner's Manual Kindle Edition
As part of their introduction to a bariatric program most patients are taught the Four Rules, which tend to be consistent from one bariatric program to the next. Many patients agree to follow the Four Rules which will work in concert with their surgically altered stomach and digestive system to bring about rapid massive weight loss. Some patients mistakenly believe they can return to the eating and lifestyle habits they practiced before surgery once they have lost the desired amount of weight. However, patients who return to their pre-surgery lifestyle and diet often fail to achieve full body fat loss and frequently regain much of the weight they initially lost.
For patients to lose all of their excess weight and maintain that weight loss they must follow the Four Rules for the rest of their life. Before undergoing any surgical procedure for weight management one must be fully aware of the Four Rules and willing to commit to them for life. Below is a quick look at each rule as it applies to WLS patients:
 | ||
| Get this infograph here: Four RULES |
Lots of Water: Like most weight loss programs, bariatric surgery patients are instructed to drink lots of water throughout the day. Water hydrates the organs and cells and facilitates the metabolic processes of human life. Water flushes toxins and waste from the body. Patients are prohibited carbonated beverages and advised to drink caffeinated or alcoholic beverages sparingly.
No Snacking: Patients are discouraged from snacking which may prevent weight loss and lead to weight gain. Specifically, patients are forbidden to partake of traditional processed carbohydrate snacks, such as chips, crackers, baked goods, and sweets. Patients who return to snacking or grazing defeat the restrictive nature of the surgery and weight gain results.
Daily Exercise: Patients in recovery from morbid obesity must increase their daily activity and progress to formal fitness building activities that include aerobic conditioning and muscular strength and endurance. Walking, swimming, and biking are all encouraged following gastric surgery. Patients who continue to follow an exercise routine will sustain weight loss and live healthier lives. Patients who do not include exercise as part of their bariatric weight loss program will most likely regain weight and suffer from co-morbidities they hoped to relieve with surgical weight loss.
Nearly a half-million Americans this year will undergo some form of bariatric surgery for the treatment of their morbid obesity. Surgical intervention is proven to be the best treatment for many people in affecting long term weight loss and weight management. However, surgery does not work alone. Patients who are compliant with the Four Rules of dietary and lifestyle change are most likely to enjoy improved health and mobility following a bariatric intervention.
Learn more about the Four Rules and get back to the basics of WLS with the 5 Day Pouch Test plan. Check out the Owner's Manual available for instant download on Kindle:
5DPT Owner's Manual Kindle Edition
Today Inspired: Monsters Under the Rug
(I posted this in our Project2014 Group and
I'm sharing it here because I know so many of my friends are
KeepHerKitty fans. I hope you enjoy this little look into KeepHer's
world of the CAT-egoricly insane!)
Today Inspired - Happy Monday Members! My Today Inspired comes from KeepHerKitty - it's a bit of a stretch, so work with me here. KeepHer is my little calico cat, assistant and best buddy. Since last winter she's been obsessed with the bathroom rug and we started playing this game called "Monsters Under the Rug - Who You Gonna Call? KeepHer Kitty!" She enthusiastically attacks the rug or runs in fear of what is under the rug. She became so obsessed with monsters that she would get me up in the night over her imaginary fears of battles with the rug. I couldn't take it anymore. That cat was crazy! So I took the rug out and a calm has returned to the bathroom. No more rug under which to hide, no more monsters: fears abated.
So here's the leap. Sometimes the problem isn't the monsters, the problem is the rug that is hiding them. Sometimes the problem is the barrier that hides the unknown. So get rid of the rug and remove the barrier. Face down the monsters. Maybe they aren't even there.
Who you gonna call? KEEPHER - KeepHerKitty!
(said to the Ghost Busters jingle).
See more of KeepHerKitty on my Pinterest Board: KeepHerKitty and on my sister blog, Crafting with Kaye.
Today Inspired - Happy Monday Members! My Today Inspired comes from KeepHerKitty - it's a bit of a stretch, so work with me here. KeepHer is my little calico cat, assistant and best buddy. Since last winter she's been obsessed with the bathroom rug and we started playing this game called "Monsters Under the Rug - Who You Gonna Call? KeepHer Kitty!" She enthusiastically attacks the rug or runs in fear of what is under the rug. She became so obsessed with monsters that she would get me up in the night over her imaginary fears of battles with the rug. I couldn't take it anymore. That cat was crazy! So I took the rug out and a calm has returned to the bathroom. No more rug under which to hide, no more monsters: fears abated.
So here's the leap. Sometimes the problem isn't the monsters, the problem is the rug that is hiding them. Sometimes the problem is the barrier that hides the unknown. So get rid of the rug and remove the barrier. Face down the monsters. Maybe they aren't even there.
Who you gonna call? KEEPHER - KeepHerKitty!
(said to the Ghost Busters jingle).
See more of KeepHerKitty on my Pinterest Board: KeepHerKitty and on my sister blog, Crafting with Kaye.
Thursday, August 07, 2014
5DPT Q&A: Quitting Carbs is Hard!
I have seen several online discussions lately about the difficulty of giving up a processed carb snacking habit. In response to that conversation I've pulled this article from our 5 Day Pouch Test Bulletin archive. Transitioning our diet from simple carbs to processed carbs is not a simple matter of will power. There are powerful biological forces at work making this a difficult, but not impossible, endeavor. Read the article below.
For more FAQ's from our bulletin link here: 5DPT Bulletin January 2014
For more FAQ's from our bulletin link here: 5DPT Bulletin January 2014
Q: Why can't I just quit carbs cold turkey without the 5DPT?
Blame it on your biology

Have
you ever had a particularly bad snacking day only to find yourself the
next morning promising to give-up snacky-carbs for good, cold turkey,
right now. And by noon that will-power is forgotten as you reach for the
snack of choice. And then the self-blame begins: "Why am so weak? Why
am I a failure? Why don't I have will-power?" I've lived this scenario
more times than I care to admit and I know I'm not alone.
But
it turns out we aren't just a bunch of weak-bellied carb-addicts. There
is a biological reason that motivates the reach for the snack: our body
has become accustomed to digesting and using processed carbs as it's
primary source of fuel. Withdrawing them cold turkey puts the metabolic
process in panic and serotonin levels drop. "You may be powerless to
resist baked goods, pasta, and their carb cousins," according to Wurtman
and Marquis in "The Serotonin Power Diet. "The reason for this
specific, very tough-to-ignore craving for carbohydrates is that your
brain is forcing you to yearn for them so that it can produce
serotonin."
With
the 5 Day Pouch Test we methodically transition from fatty
non-nutritional processed carbs to healthy complex carbohydrates found
in grains, vegetables, and fruits. The body still produces serotonin
from these carbs while benefiting from the healthy nutrients and fiber
missing from processed carbs. While some cravings for carbs are
experienced the biological trauma is not as severe as when processed
carbs are withdrawn cold turkey without providing a similar replacement
fuel.For more FAQ's from our bulletin link here: 5DPT Bulletin January 2014
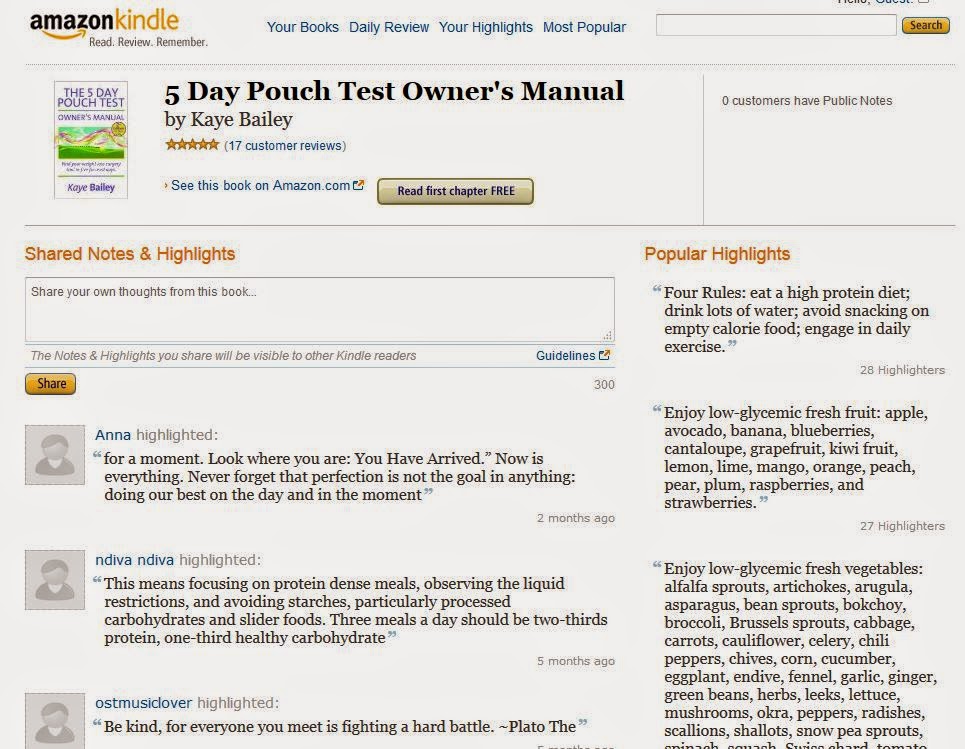
Lots of Stars and Highlights
The 5 Day Pouch Test Owner's Manual - 2nd Edition continues to be a LivingAfterWLS favorite publication. On Amazon the 5-Star ratings are adding up and Kindle readers are sharing their favorite quotes through the highlights. Check out what folks are sharing here:
5 Day Pouch Test Owner's Manual on Amazon
5 Day Pouch Test Owner's Manual on Amazon
Tuesday, August 05, 2014
Heat it up with Ginger: Delicious & Healthy Flavor
From our Cooking with Kaye Archives:
Today we celebrate the health and healing powers of ginger. Aromatic, pungent and spicy, ginger adds a special flavor and zest to main dishes and many fruit and vegetable dishes. Ginger has long been known to tame digestive discomfort and many post-weight loss surgery patients report that including ginger as an ingredient in their healthy diet helps reduce stomach distress.
Ginger can be found in many forms including fresh roots, powder, crystallized, candied and pickled. For the best healing properties select fresh ginger root found in the produce section of your market. Fresh ginger should be refrigerated unpeeled. For use in cooking peel the ginger, a potato peeler works well, and chop, slice or mince as directed.
Ginger Chicken
This recipe will remind of your favorite Chinese takout. The marinade turns up the heat on the same 'ole chicken breast. As written the recipe calls for cooked rice but many weight loss surgery patients do not tolerate rice. We served it over baby spinach greens and it was delicious!
Ingredients:
1/3 cup low-sodium soy sauce
1/4 cup orange juice
3 tablespoons finely chopped green onions
1 tablespoon grated peeled fresh ginger
1 tablespoon lemon juice
1 tablespoon honey
1 teaspoon dried basil
1/2 teaspoon pepper
1/4 teaspoon crushed red pepper (1/4 to 1/2 teaspoon)
1/4 teaspoon five-spice powder
4 garlic cloves, minced
1 pound skinned boned chicken breasts, cut into 1/2-inch-wide strips
2 teaspoons vegetable oil
4 cups hot cooked rice (optional)
Directions: Combine first 12 ingredients in a bowl; stir well. Cover and marinate in refrigerator 30 minutes. Drain chicken, reserving marinade. Heat oil in a large nonstick skillet over medium heat. Add chicken; sauté 5 minutes. Add reserved marinade; cover, reduce heat, and simmer 5 minutes. Serve over rice.
Serving Size: 3 ounces chicken and 1 cup rice. Per serving: 430 calories, 33 grams protein, 4 frams fat (1 saturated), 62 grams carbohydrate and 1 gram dietary fiber.
Without rice: 190 calories. 28 grams protein, 4 grams fat (1 saturated), 10 grams carbohydrate adn 1 gram dietary fiber.
Link to this archived newsletter:
Cooking with Kaye - Heat it up with Ginger
Please note offers and promotions in this 2007 newsletter have expired and will not be honored. For current special offers and sales of LivingAfterWLS products and publications visit the LivingAfterWLS General Store.
Monday, August 04, 2014
Project 2014: Season III Begins!
LivingAfterWLS Project 2014
Season III: Summer
Living well and empowered
Living well and empowered

Welcome to Season III - Summer of our LivingAfterWLS Project 2014. I am so pleased you have joined me for this exciting and meaningful approach to health and weight management using our weight loss surgery tool empowered by our collective knowledge and strength. We continued to pursue our goal in Season II - Spring to unite like-minded people through education, support, and lasting health sustainability using our surgical tool for weight loss and weight management. Our Facebook group grew to over 1200 members and we enjoy lively and supportive conversation daily. We listened to feedback from our membership and have revamped our units and worksheets for Season III to feel less like homework and more like engaging fun. You will notice these changes beginning in Unit II. Like our other seasons, Unit 1 of Summer is the activity of completing the Personal Self-Assessment and making daily entries in our Today Inspired micro-diary. The worksheets are attached in this convenient PDF download.
We hope you love the new worksheets and find them useful tools in the ongoing pursuit of good health and weight management with weight loss surgery. As always we remain committed to our goal of uniting like-minded people through education, support, and community, while promoting health sustainability and weight management with weight loss surgery.
Season III: Unit 1:
Personal Empowerment - You are in control.
Download Season III Unit 1Personal Empowerment - You are in control.
Personal Responsibility: Our best weapon against biology and environment WLS patients have a tremendous sense of personal responsibility in controlling their health through weight management with surgery. In summarizing the research on biology and environment in relation to obesity expert George Bray said, "Genes load the gun, the environment pulls the trigger." No wonder we struggle, even with surgical intervention, in the fight against obesity. Dr. Brownell attaches great hope to personal responsibility saying, "Calling on people to make better decisions and providing them with the skills to do so should always be the first step, always the default. This is consistent with our country's character and also with psychological principles; people who change through their own efforts have enhanced self-esteem and maintain the changes longer."
Link to Newsletter
Subscribe to:
Posts (Atom)